TCTAP C-183
| ENDOVASCULAR - Peripheral Vascular Disease and Intervention | |
| How to Manage Spontaneous Renal Artery Dissection (SRAD) Better? | |
| Chieh-yu Chen1, Jen-Kuang Lee1 | |
| National Taiwan University Hospital, Taiwan1, | |
| JACC | |
|
[Clinical Information]
- Patient initials or identifier number:
SRAD case
-Relevant clinical history and physical exam:
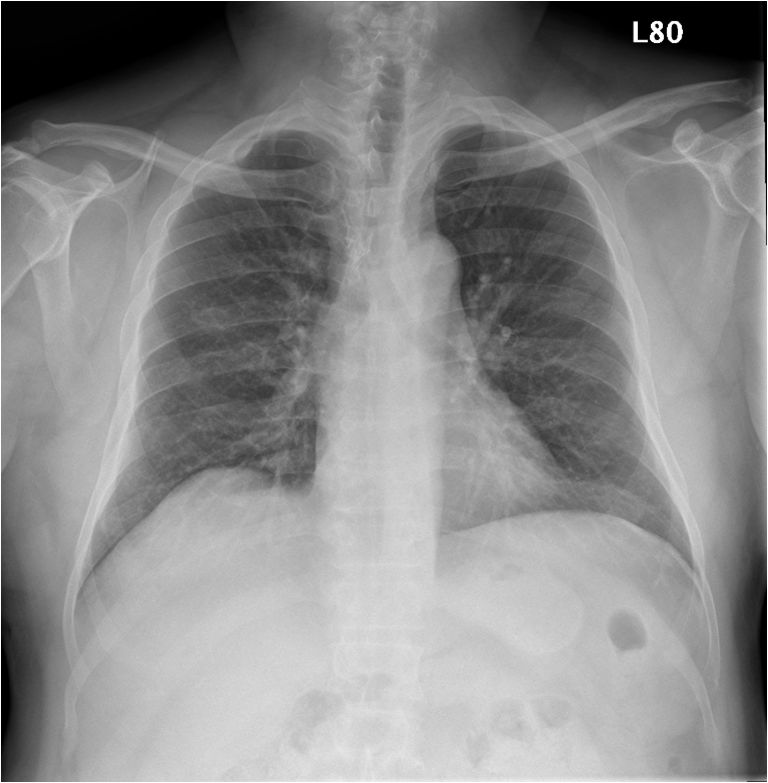
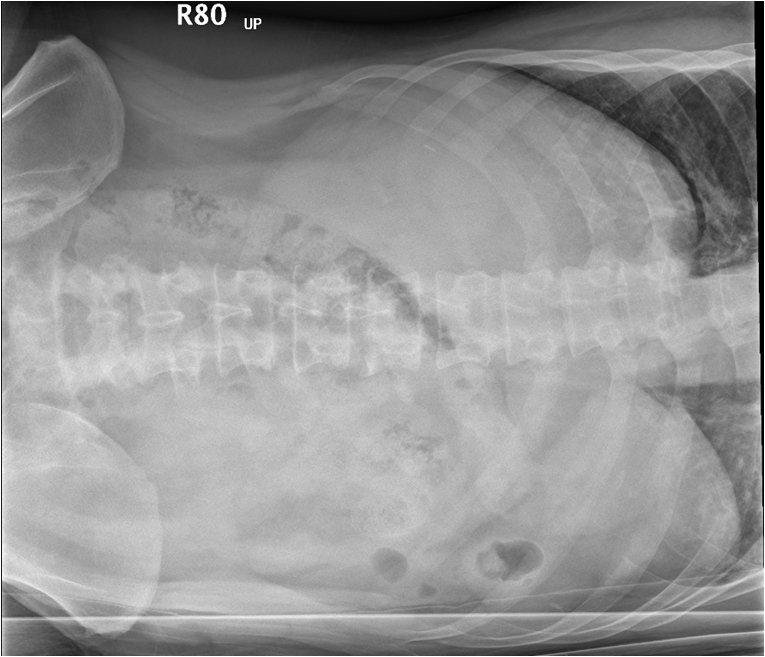
This 49-year-old man with the history of mediastinal Hodgkin lymphoma after treatment in complete remission status presented with sudden onset of left lower abdominal pain for one day, and with no known trauma history. Chest radiography showed no active lung lesion and no subphrenic free air. Flat abdomen and lateral decubitus KUB views also revealed no evidence of free air.
   -Relevant test results prior to catheterization:
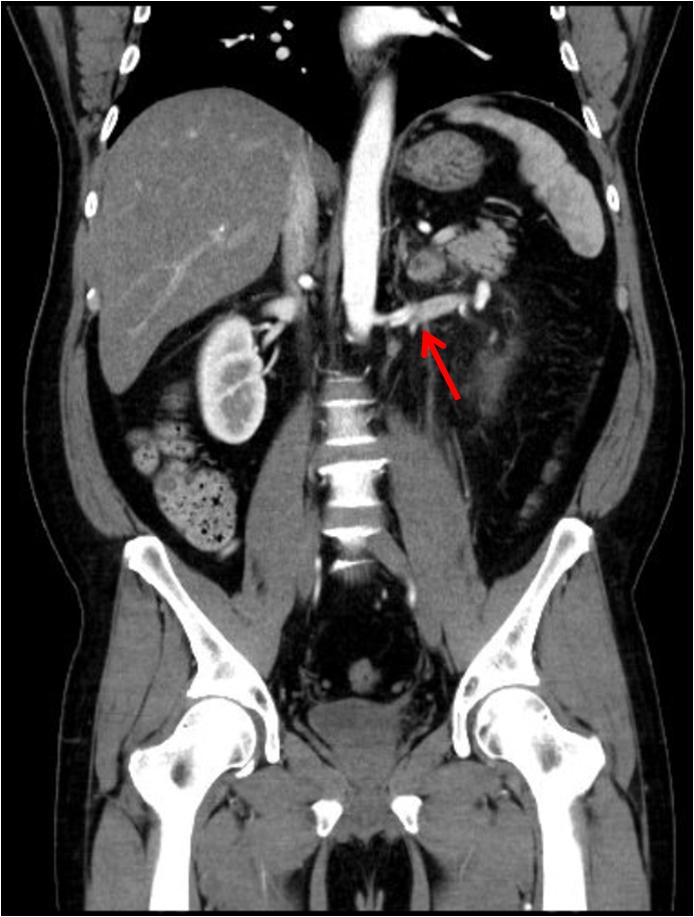
Abdominal CT scan yielded left renal artery spontaneous dissection with renal infarction.
   - Relevant catheterization findings:
Fluoroscopic angiography showed the findings compatible with the CT scan, which revealed the two dissection flaps were located from the main trunk of left renal artery to the segmental branch with pseudoaneurysm formation, and we decided to do endovascular revascularization after discussion.
|
|
|
[Interventional Management]
- Procedural step:
First,we engaged Boston RDC 7 Fr. guiding catheter to the left renal artery, wiring Abbott BMW ELITE wire with CXI 2.6 Fr. microcatheter support to one of the inferior segmental branch of left renal artery across the dissection region. IVUS confirmed the wire in the distal true lumen of the dissection. Due to distal portion of the dissection adjacent to abundant branches of renal artery, a fenestrated stent was of the choice to avoid branch compromise; proximal portion of the dissection locating on the main trunk was favored for a covered stent as our intervention strategy. We inserted additional ASAHI Fielder FC wire to the distal true lumen for buddy wire support. Balloon angioplasty (BA) was then performed to the distal dissection portion with Medtronic Sprinter 3*12 mm balloon, and theballoon-expandable, fenestrated stent “Abbott MULTI-LINK 4*38 mm”was deployed to cover the distal dissection flap. After the first stenting, Boston V-18 0.018” 300 cm, and another Abbott MULTI-LINK 4*28 mm stent was implanted; however, the stent shortening was found, another balloon-expandable, fenestrated stent “Medtronic Assurant Cobalt7*30 mm” was then deployed to the remaining dissection portion adjacent to the branch openings, and post-dilatation was also done for optimal luminal size. The last self-expandable covered stent “GORE Viabahn Endoprosthesis 6*50 mm” was implanted at the proximal dissection portion as well as coverage of pseudoaneurysm of the left renal artery main trunk.
- Case Summary:
After fenestrated and covered stenting, good flow of the left renal artery was noted with better renal perfusion via angiography, and IVUS also confirmed well apposition of the stents. The patient’s symptom was gradually improved later. In this case, we learned about the following importance: (1) identify the candidate of endovascular revascularization, (2) make sure successful wiring skill to the distal true lumen of the dissection with the aid of necessary devices, (3) decide the landing zone of stenting and stent types, (4) check final better renal perfusion, and (5) know the etiology of spontaneous renal artery dissection and how to manage it better, including other feasible strategies.
|
|