News | SummitMD
FFR-guided PCI fails to show noninferiority against CABG in triple-vessel CAD: FAME 3
Surgery comes out ahead, but both CABG, PCI see improvements over past studies; sub-analysis suggests SYNTAX score helps choose best revasc strategy
Patients with triple-vessel coronary artery disease (CAD) fared better with open-heart surgery than fractional flow reserve (FFR)-guided stenting at 1-year, but both revascularization strategies showed improvements over the past decade, latest study findings showed.
In the FAME 3 study, FFR-guided percutaneous coronary intervention (PCI) with second-generation drug-eluting stents (DES) failed to prove noninferiority compared to coronary artery bypass grafting (CABG) for the composite primary endpoint of major adverse cardiac and cerebrovascular events (MACCE) at 1-year (FFR-PCI: 10.6% vs. CABG 6.9%; HR 1.5, 95% CI, 1.1-2.2).
However, subgroup analysis showed that patients with low SYNTAX scores (<23) undergoing FFR-guided PCI had numerically, but not statistically significant, lower rates of MACCE than those receiving CABG - indicating that SYNTAX scores could play a role in narrowing down a revascularization strategy for optimal outcomes.
1-year MACCE rates based on SYNTAX score: FAME 3
SYNTAX score
PCI
CABG
0-22
5.5%
8.6%
23-32
13.7%
6.1%
≥33
12.1%
6.6%
“CABG had a lower incidence of the composite of death, myocardial infarction (MI), stroke, or repeat revascularization at 1-year than FFR-guided PCI with current-generation zotarolimus-eluting stents,” FAME 3 investigators wrote in the New England Journal of Medicine (NEJM) paper published on Nov 4 last year[1]. “The incidence of the secondary composite endpoint of death, MI, or stroke and each component of the primary endpoint did not differ significantly between the two groups.”
Principal investigator William Fearon, MD (Stanford University School of Medicine, California, USA) - simultaneously presenting study findings at the virtual TCT 2021 conference - said: “Bypass surgery remains the treatment of choice in more complex disease, but FFR-guided PCI is a reasonable option for lower complexity, based on the SYNTAX score.”
“The good news is that treatment of multivessel disease has improved dramatically for both FFR-guided stenting and bypass surgery. Both performed markedly better than historical controls,” he said.
Fearon highlighted that the team would continue with 3- and 5-year follow-up to assess long-term outcomes of the two strategies to mend the limitation of the short 1-year follow-up.
Ran Kornowski, MD (Rabin Medical Center, Petah Tikva, Israel), session panelist at TCT 2021, said: “The main message for three-vessel CAD is that FFR-guided PCI produces good results, but surgery does better. We need more data on long-term outcomes beyond one year and the completeness of revascularization based on FFR measurements. Sub-analysis on SYNTAX scores provides important data for clinical decision making with patients.”
Bypass surgery remains the treatment of choice in more complex disease, but FFR-guided PCI is reasonable in less complex disease, depending on the SYNTAX score.
Evolution of PCI calls for updated trials comparing FFR versus angiography guidance and CABG
The advent of new technologies and technical progress on both sides of the revascularization spectrum called for head-to-head trials comparing PCI and CABG in the same patient population.
Previous studies on triple-vessel CAD had demonstrated that CABG outperformed PCI for clinical outcomes, serving as the foundation for US and European guidelines to recommend CABG for most patients.
The 2018 European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) joint guideline on myocardial revascularization[2] strongly recommended CABG for triple-vessel CAD regardless of the SYNTAX score (Class Ia). The European guideline advised against PCI for triple-vessel CAD patients with an intermediate-to-high SYNTAX score ≥22 (Class IIIa) and limited stenting to triple-CAD with only low SYNTAX scores (≤22) and no diabetes (Class Ia).
The 2021 American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) joint guideline on coronary artery revascularization[3] downgraded both CABG and PCI to a Class IIb for patients with triple-vessel disease and normal ejection fraction with or without proximal left anterior descending (LAD). The guideline noted that surgery might be “reasonable” to lower mortality risk. The survival benefit with PCI was “uncertain,” requiring heart team deliberations on disease complexity and technical feasibility of treatment.
The FAME 3 trial incorporated updates in the revascularization landscape to compare stenting versus open-heart surgery in triple-vessel CAD considering most previous studies had either used bare-metal stents (BMS) or first-generation DES, and none incorporated the FFR index.
Before FAME 3, the first FAME trial in 2009[4] showed FFR-guided PCI slashed risks of all-cause mortality, MI, and repeat revascularization versus angiography-guided PCI. The FAME 2 trial in 2012[5] showed the superiority of FFR-guided PCI and medical therapy over medical therapy alone for stable ischemic heart disease.
Surgery defends ‘famed’ golden crown with lower MACCE rates in 3-vessel CAD
The investigator-initiated, multicenter, international, noninferiority, randomized controlled FAME 3 trial enrolled 1,500 patients (avg age: 65; 82% male) at 48 centers to undergo either PCI (n=757, mean lesions: 4.3, mean stents: 3.7±1.9) or CABG (n=743; mean lesions: 4.2 lesions; mean distal anastomosis: 3.4±1.0).
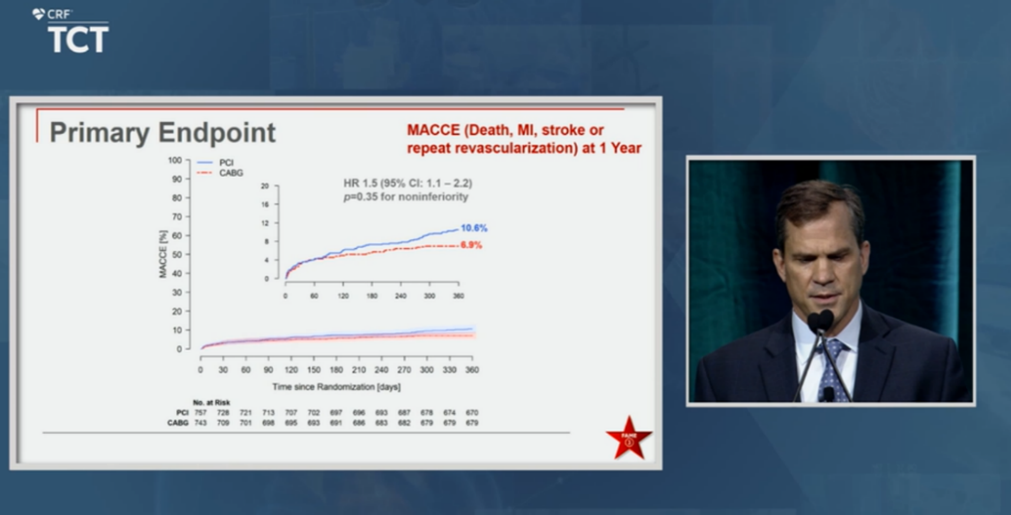
William Fearon, MD presents FAME 3 findings at TCT 2021 on Nov 4, 2021 ©2021 CRF
The primary 1-year endpoint was MACCE - defined as death from any cause, MI, stroke, or repeat revascularization. Secondary endpoints were composite of death, MI, or stroke.
Key inclusion criteria included patients with triple-vessel CAD defined as ≥50% diameter stenosis in three major epicardial vessels and amenable by revascularization by PCI or CABG. Primary exclusion criteria included recent STEMI (within five days), cardiogenic shock, and left ventricular ejection fraction (LVEF)<30%.
Noninferiority margins were initially prespecified to 1.45 (95% CI) but later raised to an upper boundary of less than 1.65 (95% CI) in light of recently published data. Fearon noted that this made it “harder to achieve noninferiority compared to absolute values since the absolute difference dropped after the CABG arm demonstrated lower than anticipated MACCE rates.”
The main message for three-vessel CAD is that FFR-guided PCI produces good results, but surgery does better.
Results showed a higher occurrence of the composite primary endpoint in the PCI arm, indicating FFR-guided PCI failed to prove noninferiority to CABG (FFR-PCI: 10.6% vs. CABG 6.9%; HR 1.5, 1.1-2.2).
Incidence of death, MI, or stroke was also higher with FFR-guided PCI (7.3% vs. 5.2%; HR 1.4, 0.9-2.1), although the difference was not statistically significant.
For safety outcomes, CABG reported higher incidence of major bleeding defined as BARC type 3-5 (FFR-PCI: 1.6% vs. CABG: 3.8%, p<0.01), atrial fibrillation/arrhythmia (2.4% vs. 14.1%, p<0.001), and acute kidney injury (0.1% vs. 0.9%, p<0.04).
Despite the flopped test of noninferiority, FFR-guided PCI proved to be a “very reasonable option” for triple-vessel CAD, particularly for patients with lower SYNTAX scores, Fearon said. Both arms showed considerable improvements over time and compared to the first SYNTAX trial[6].
Fearon pointed out that both FAME 3 and SYNTAX had similar patient baseline characteristics, but analysis showed that 1-year MACCE rates improved significantly in FAME 3 (SYNTAX vs. FAME 3: PCI rates 17.8% vs. 10.6%; CABG rates: 12.4% vs. 6.9%). Notably, both the FFR-guided PCI and CABG arms in FAME 3 outperformed the surgical arm of the SYNTAX trial.
“Although these trials are not directly comparable, patients assigned to undergo PCI in FAME 3 also had a lower incidence of repeat revascularization (4.9% vs. 13.5%) and lower mortality (1.6% vs. 4.4%) than the SYNTAX trial, despite having similar patient characteristics and risk profiles,” researchers wrote. “Plausible explanations for these findings include improved stent technology, high medical treatment adherence, and fewer stents implanted that lowered the risk of stent-related complications.”
CABG may be preferred when FFR measurements show functional triple-vessel CAD, but PCI remains a feasible option when FFR-guidance shows functional single- or double-vessel CAD.
Effectiveness of FFR-guidance over angiography-guidance called into question
Although Fearon stressed the collective improvement in outcomes for both arms compared to previous trials, cardiac surgeon and TCT session panelist Mario F.L. Gaudino, MD (Weill Cornell Medicine, New York, USA) pointed out that FFR-guidance did not show significant progress compared to the more recent NOBLE and EXCEL trials – reiterating bypass surgery as the golden standard.
“Comparing FAME 3 to SYNTAX, which was conducted over ten years ago, does not make sense,” Gaudino said. “When comparing outcomes to the contemporary NOBLE[7][8] and EXCEL[9] trials (since FAME 3 did not have an angio-guided arm for comparison), we see no improvement in PCI outcomes. Superiority of FFR-guidance over angiography for stenting was the primary underlying hypothesis of FAME 3.”
Gaudino pointed out that the FARGO trial[10], which examined outcomes between angiography- and FFR-guided CABG, found a “concerning” accelerated progression of lesions with FFR-guidance, demonstrating that patients with less severe CAD derive less benefit with FFR than those with severe disease. The FLOWER-MI trial[11][12] published in July also showed that FFR-guided PCI did not reduce the risk of primary endpoint occurrence compared to angio-guided PCI.
Jung-Min Ahn, MD (Asan Medical Center, Seoul, South Korea) told SummitMD that the study reaffirmed CABG superiority over PCI for patients with severe CAD but pointed out key considerations for applying findings to the clinical setting.
“In the FFR-guided PCI arm of FAME 3, FFR was not measured in 18% of lesions mostly due to subtotal or total occlusion, and only 24% of lesions intended for treatment had FFR measurements greater than 0.80,” Ahn said. “It follows that FFR-measurements may not have played a big role in choosing the revascularization strategy in the study and most patients in FAME 3 may have had functional triple-vessel CAD.”
“Then it’s inevitable that FAME 3 results paralleled outcomes from the BEST study published in the NEJM in 2015 - which hinged on decision-making with angio-guidance - indicating that we cannot properly understand FAME 3 without taking these factors into account,” Ahn said. “The takeaway is that CABG may be preferred when FFR measurements show functional triple-vessel CAD, but PCI remains a feasible option when FFR-guidance shows functional single- or double-vessel CAD.”
- https://www.nejm.org/doi/full/10.1056/NEJMoa2112299
- https://academic.oup.com/eurheartj/article/40/2/87/5079120
- https://www.jacc.org/doi/10.1016/j.jacc.2021.09.005
- https://www.nejm.org/doi/full/10.1056/nejmoa0807611
- https://www.nejm.org/doi/full/10.1056/nejmoa1205361
- https://www.nejm.org/doi/full/10.1056/nejmoa0804626
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)32052-9/fulltext
- https://www.thelancet.com/article/S0140-6736(19)32972-1/fulltext
- https://www.nejm.org/doi/full/10.1056/nejmoa1909406
- https://www.jacc.org/doi/10.1016/j.jacc.2018.09.043
- https://www.nejm.org/doi/full/10.1056/NEJMoa2104650
- https://www.summitmd.com/html/technical/news_view.php?cmode=daily&no_case=86&part=c
Edited by

Jung-Min Ahn , MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read Biography
Patients with triple-vessel coronary artery disease (CAD) fared better with open-heart surgery than fractional flow reserve (FFR)-guided stenting at 1-year, but both revascularization strategies showed improvements over the past decade, latest study findings showed.
In the FAME 3 study, FFR-guided percutaneous coronary intervention (PCI) with second-generation drug-eluting stents (DES) failed to prove noninferiority compared to coronary artery bypass grafting (CABG) for the composite primary endpoint of major adverse cardiac and cerebrovascular events (MACCE) at 1-year (FFR-PCI: 10.6% vs. CABG 6.9%; HR 1.5, 95% CI, 1.1-2.2).
However, subgroup analysis showed that patients with low SYNTAX scores (<23) undergoing FFR-guided PCI had numerically, but not statistically significant, lower rates of MACCE than those receiving CABG - indicating that SYNTAX scores could play a role in narrowing down a revascularization strategy for optimal outcomes.
| 1-year MACCE rates based on SYNTAX score: FAME 3 | ||
|---|---|---|
| SYNTAX score | PCI | CABG |
| 0-22 | 5.5% | 8.6% |
| 23-32 | 13.7% | 6.1% |
| ≥33 | 12.1% | 6.6% |
“CABG had a lower incidence of the composite of death, myocardial infarction (MI), stroke, or repeat revascularization at 1-year than FFR-guided PCI with current-generation zotarolimus-eluting stents,” FAME 3 investigators wrote in the New England Journal of Medicine (NEJM) paper published on Nov 4 last year[1]. “The incidence of the secondary composite endpoint of death, MI, or stroke and each component of the primary endpoint did not differ significantly between the two groups.”
Principal investigator William Fearon, MD (Stanford University School of Medicine, California, USA) - simultaneously presenting study findings at the virtual TCT 2021 conference - said: “Bypass surgery remains the treatment of choice in more complex disease, but FFR-guided PCI is a reasonable option for lower complexity, based on the SYNTAX score.”
“The good news is that treatment of multivessel disease has improved dramatically for both FFR-guided stenting and bypass surgery. Both performed markedly better than historical controls,” he said.
Fearon highlighted that the team would continue with 3- and 5-year follow-up to assess long-term outcomes of the two strategies to mend the limitation of the short 1-year follow-up.
Ran Kornowski, MD (Rabin Medical Center, Petah Tikva, Israel), session panelist at TCT 2021, said: “The main message for three-vessel CAD is that FFR-guided PCI produces good results, but surgery does better. We need more data on long-term outcomes beyond one year and the completeness of revascularization based on FFR measurements. Sub-analysis on SYNTAX scores provides important data for clinical decision making with patients.”
Bypass surgery remains the treatment of choice in more complex disease, but FFR-guided PCI is reasonable in less complex disease, depending on the SYNTAX score.
Evolution of PCI calls for updated trials comparing FFR versus angiography guidance and CABG
The advent of new technologies and technical progress on both sides of the revascularization spectrum called for head-to-head trials comparing PCI and CABG in the same patient population.
Previous studies on triple-vessel CAD had demonstrated that CABG outperformed PCI for clinical outcomes, serving as the foundation for US and European guidelines to recommend CABG for most patients.
The 2018 European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) joint guideline on myocardial revascularization[2] strongly recommended CABG for triple-vessel CAD regardless of the SYNTAX score (Class Ia). The European guideline advised against PCI for triple-vessel CAD patients with an intermediate-to-high SYNTAX score ≥22 (Class IIIa) and limited stenting to triple-CAD with only low SYNTAX scores (≤22) and no diabetes (Class Ia).
The 2021 American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) joint guideline on coronary artery revascularization[3] downgraded both CABG and PCI to a Class IIb for patients with triple-vessel disease and normal ejection fraction with or without proximal left anterior descending (LAD). The guideline noted that surgery might be “reasonable” to lower mortality risk. The survival benefit with PCI was “uncertain,” requiring heart team deliberations on disease complexity and technical feasibility of treatment.
The FAME 3 trial incorporated updates in the revascularization landscape to compare stenting versus open-heart surgery in triple-vessel CAD considering most previous studies had either used bare-metal stents (BMS) or first-generation DES, and none incorporated the FFR index.
Before FAME 3, the first FAME trial in 2009[4] showed FFR-guided PCI slashed risks of all-cause mortality, MI, and repeat revascularization versus angiography-guided PCI. The FAME 2 trial in 2012[5] showed the superiority of FFR-guided PCI and medical therapy over medical therapy alone for stable ischemic heart disease.
Surgery defends ‘famed’ golden crown with lower MACCE rates in 3-vessel CAD
The investigator-initiated, multicenter, international, noninferiority, randomized controlled FAME 3 trial enrolled 1,500 patients (avg age: 65; 82% male) at 48 centers to undergo either PCI (n=757, mean lesions: 4.3, mean stents: 3.7±1.9) or CABG (n=743; mean lesions: 4.2 lesions; mean distal anastomosis: 3.4±1.0).
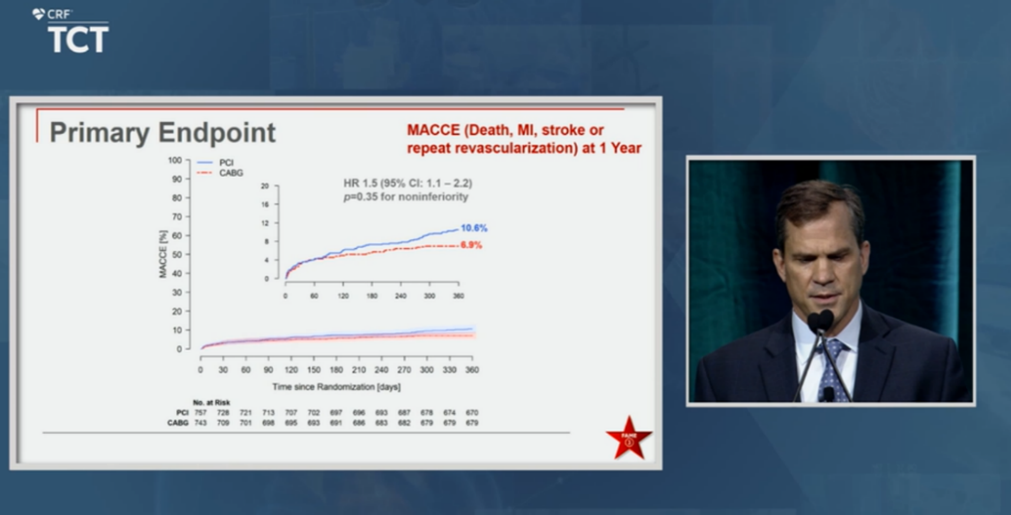
William Fearon, MD presents FAME 3 findings at TCT 2021 on Nov 4, 2021 ©2021 CRF
The primary 1-year endpoint was MACCE - defined as death from any cause, MI, stroke, or repeat revascularization. Secondary endpoints were composite of death, MI, or stroke.
Key inclusion criteria included patients with triple-vessel CAD defined as ≥50% diameter stenosis in three major epicardial vessels and amenable by revascularization by PCI or CABG. Primary exclusion criteria included recent STEMI (within five days), cardiogenic shock, and left ventricular ejection fraction (LVEF)<30%.
Noninferiority margins were initially prespecified to 1.45 (95% CI) but later raised to an upper boundary of less than 1.65 (95% CI) in light of recently published data. Fearon noted that this made it “harder to achieve noninferiority compared to absolute values since the absolute difference dropped after the CABG arm demonstrated lower than anticipated MACCE rates.”
The main message for three-vessel CAD is that FFR-guided PCI produces good results, but surgery does better.
Results showed a higher occurrence of the composite primary endpoint in the PCI arm, indicating FFR-guided PCI failed to prove noninferiority to CABG (FFR-PCI: 10.6% vs. CABG 6.9%; HR 1.5, 1.1-2.2).
Incidence of death, MI, or stroke was also higher with FFR-guided PCI (7.3% vs. 5.2%; HR 1.4, 0.9-2.1), although the difference was not statistically significant.
For safety outcomes, CABG reported higher incidence of major bleeding defined as BARC type 3-5 (FFR-PCI: 1.6% vs. CABG: 3.8%, p<0.01), atrial fibrillation/arrhythmia (2.4% vs. 14.1%, p<0.001), and acute kidney injury (0.1% vs. 0.9%, p<0.04).
Despite the flopped test of noninferiority, FFR-guided PCI proved to be a “very reasonable option” for triple-vessel CAD, particularly for patients with lower SYNTAX scores, Fearon said. Both arms showed considerable improvements over time and compared to the first SYNTAX trial[6].
Fearon pointed out that both FAME 3 and SYNTAX had similar patient baseline characteristics, but analysis showed that 1-year MACCE rates improved significantly in FAME 3 (SYNTAX vs. FAME 3: PCI rates 17.8% vs. 10.6%; CABG rates: 12.4% vs. 6.9%). Notably, both the FFR-guided PCI and CABG arms in FAME 3 outperformed the surgical arm of the SYNTAX trial.
“Although these trials are not directly comparable, patients assigned to undergo PCI in FAME 3 also had a lower incidence of repeat revascularization (4.9% vs. 13.5%) and lower mortality (1.6% vs. 4.4%) than the SYNTAX trial, despite having similar patient characteristics and risk profiles,” researchers wrote. “Plausible explanations for these findings include improved stent technology, high medical treatment adherence, and fewer stents implanted that lowered the risk of stent-related complications.”
CABG may be preferred when FFR measurements show functional triple-vessel CAD, but PCI remains a feasible option when FFR-guidance shows functional single- or double-vessel CAD.
Effectiveness of FFR-guidance over angiography-guidance called into question
Although Fearon stressed the collective improvement in outcomes for both arms compared to previous trials, cardiac surgeon and TCT session panelist Mario F.L. Gaudino, MD (Weill Cornell Medicine, New York, USA) pointed out that FFR-guidance did not show significant progress compared to the more recent NOBLE and EXCEL trials – reiterating bypass surgery as the golden standard.
“Comparing FAME 3 to SYNTAX, which was conducted over ten years ago, does not make sense,” Gaudino said. “When comparing outcomes to the contemporary NOBLE[7][8] and EXCEL[9] trials (since FAME 3 did not have an angio-guided arm for comparison), we see no improvement in PCI outcomes. Superiority of FFR-guidance over angiography for stenting was the primary underlying hypothesis of FAME 3.”
Gaudino pointed out that the FARGO trial[10], which examined outcomes between angiography- and FFR-guided CABG, found a “concerning” accelerated progression of lesions with FFR-guidance, demonstrating that patients with less severe CAD derive less benefit with FFR than those with severe disease. The FLOWER-MI trial[11][12] published in July also showed that FFR-guided PCI did not reduce the risk of primary endpoint occurrence compared to angio-guided PCI.
Jung-Min Ahn, MD (Asan Medical Center, Seoul, South Korea) told SummitMD that the study reaffirmed CABG superiority over PCI for patients with severe CAD but pointed out key considerations for applying findings to the clinical setting.
“In the FFR-guided PCI arm of FAME 3, FFR was not measured in 18% of lesions mostly due to subtotal or total occlusion, and only 24% of lesions intended for treatment had FFR measurements greater than 0.80,” Ahn said. “It follows that FFR-measurements may not have played a big role in choosing the revascularization strategy in the study and most patients in FAME 3 may have had functional triple-vessel CAD.”
“Then it’s inevitable that FAME 3 results paralleled outcomes from the BEST study published in the NEJM in 2015 - which hinged on decision-making with angio-guidance - indicating that we cannot properly understand FAME 3 without taking these factors into account,” Ahn said. “The takeaway is that CABG may be preferred when FFR measurements show functional triple-vessel CAD, but PCI remains a feasible option when FFR-guidance shows functional single- or double-vessel CAD.”
- https://www.nejm.org/doi/full/10.1056/NEJMoa2112299
- https://academic.oup.com/eurheartj/article/40/2/87/5079120
- https://www.jacc.org/doi/10.1016/j.jacc.2021.09.005
- https://www.nejm.org/doi/full/10.1056/nejmoa0807611
- https://www.nejm.org/doi/full/10.1056/nejmoa1205361
- https://www.nejm.org/doi/full/10.1056/nejmoa0804626
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)32052-9/fulltext
- https://www.thelancet.com/article/S0140-6736(19)32972-1/fulltext
- https://www.nejm.org/doi/full/10.1056/nejmoa1909406
- https://www.jacc.org/doi/10.1016/j.jacc.2018.09.043
- https://www.nejm.org/doi/full/10.1056/NEJMoa2104650
- https://www.summitmd.com/html/technical/news_view.php?cmode=daily&no_case=86&part=c
Edited by

Jung-Min Ahn , MD
Asan Medical Center, Korea (Republic of)
Written by



Leave a comment