News | TCTAP 2024
Who Will Treat the Most Complex Patients? No Success Goes Unpunished.
Live Case & Lecture 6: Complex PCI
Spencer B. King III
Emory Healthcare, USA
During TCTAP 2024, live cases, and lecture 6, the discussion revolved around the treatment of the most complex patient cases. Spencer B. King, MD (Emory University School of Medicine, Atlanta, GA, USA) shared insights into the evolving role of percutaneous coronary intervention (PCI) compared to surgery in such cases.
In his introductory remarks, King emphasized the shifting landscape of PCI being increasingly favored over surgery, particularly in treating left main (LM) shaft disease. Significant contributions by Seung-Jung Park, MD (Asan Medical Center, Seoul, Korea) were highlighted in this paradigm shift.
Previously, interventionists would often opt for surgery when confronted with challenging cases. However, King noted a trend toward choosing PCI, citing highly sophisticated PCI skills as a driving factor.
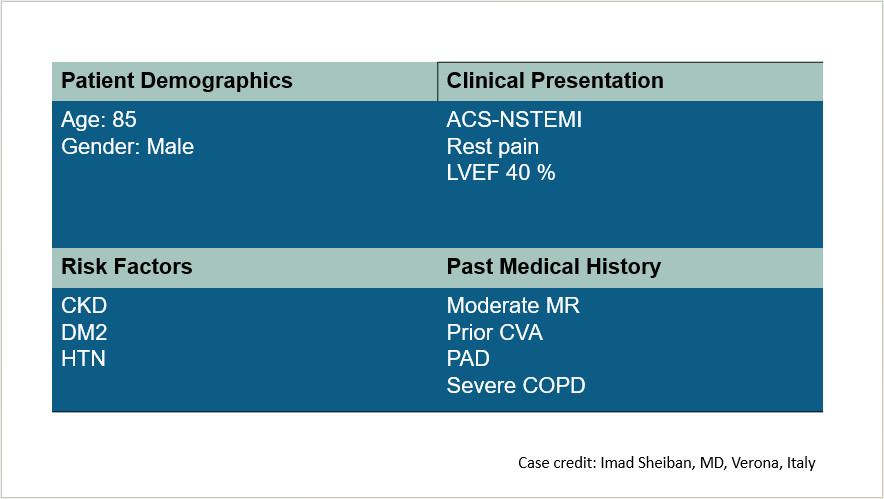
An illustrative case discussed was that of an 85-year-old male patient with a history of acute coronary syndrome (ACS), recurrent chest pain, and heart failure (Figure 1). The patient presented with multiple risk factors including diabetes, chronic renal failure, cerebrovascular accident, peripheral artery disease, and severe chronic obstructive pulmonary disease. The electrocardiogram confirmed LM disease consistent with ACS.
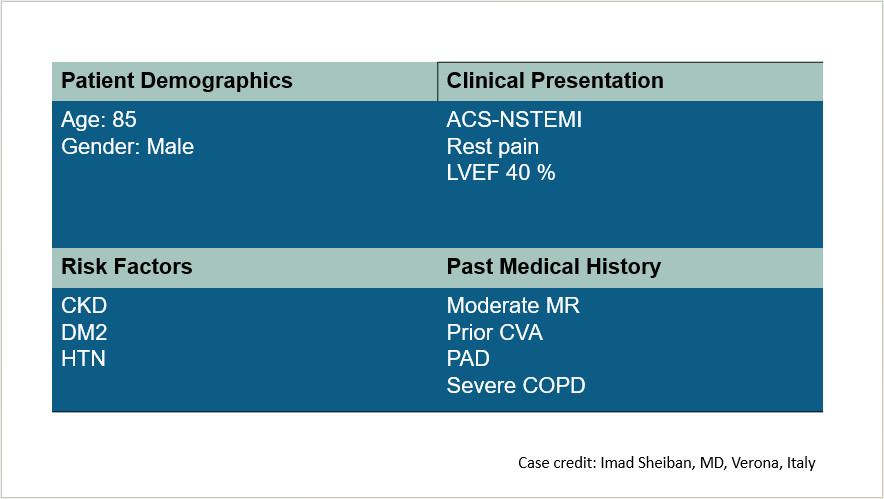
Figure 1. One most complex patient case
Initial coronary angiography revealed LM plus triple-vessel disease with complex lesions, including LM trifurcation disease and heavily calcified, diffuse long left anterior descending artery disease, alongside total occlusion of the proximal right coronary artery.
Given the patient's profile, both coronary artery bypass surgery (CABG) and PCI were considered. However, CABG was deemed prohibitive due to technical challenges, and the patient's advanced age and comorbidities. PCI posed its own difficulties, including the complexity of LM trifurcation lesions, the need for debulking procedures such as rotablation, and potential requirement for mechanical circulatory support. Assessing the postoperative outcomes, surgical mortality rates were projected to be high, prompting a thorough evaluation of the risks associated with both procedures. Ultimately, PCI was chosen for this high-risk patient, with successful completion reported.
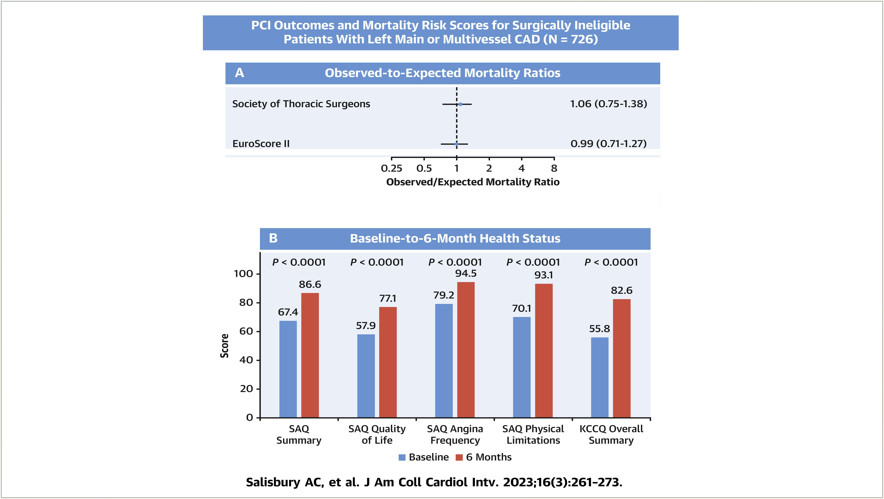
King highlighted the lack of randomized controlled trials focusing on PCI for such complex cases. Instead, he referenced a recent registry study involving over 700 patients who were turned down for surgery and underwent PCI at specialized centers. The study showed that there was no difference in the actual mortality rate compared to the mortality rate predicted by the Society of Thoracic Surgeons score and EuroScore II, and that the symptoms of the patients improved 6 months after PCI compared to the baseline condition (Figure 2).
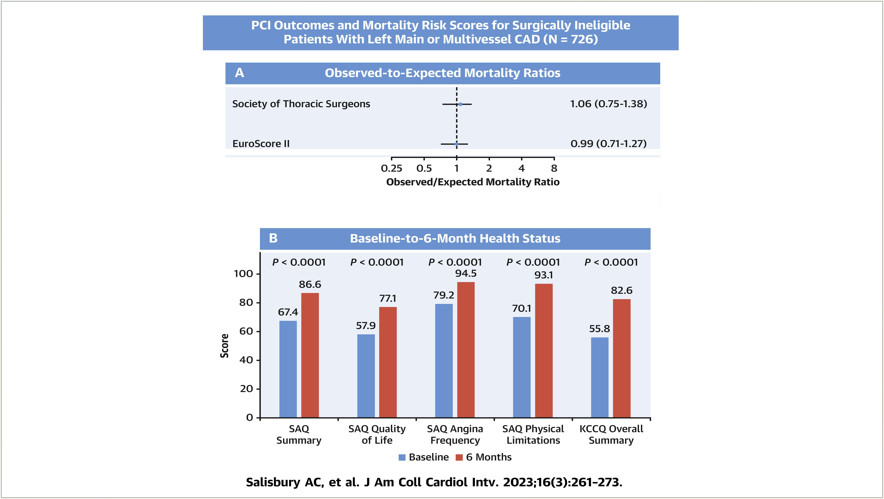
Figure 2. Improvement in patient symptoms 6 months after PCI compared to baseline condition
Looking ahead, King emphasized the need for further research to validate these findings and address key questions surrounding the selection of treatment modalities for complex cases. He advocated the establishment of local registries for high-risk patients to inform clinical decision-making.
In concluding the lecture, King left a lasting message for interventional cardiologists that no spectacular success will go unpunished and the more tough cases you take, the more you will get, which may be a good thing.
As the field continues to evolve, the quest for optimal treatment strategies for the most complex patients remains ongoing.
Live Case & Lecture 6: Complex PCI
Friday, April 26, 3:30 PM ~ 5:00 PM
Main Arena, Level 2
Edited by

Sang-Cheol Cho , MD
Yeosu Jeil Hospital, Korea (Republic of)
Spencer B. King III
Emory Healthcare, USA
During TCTAP 2024, live cases, and lecture 6, the discussion revolved around the treatment of the most complex patient cases. Spencer B. King, MD (Emory University School of Medicine, Atlanta, GA, USA) shared insights into the evolving role of percutaneous coronary intervention (PCI) compared to surgery in such cases.
In his introductory remarks, King emphasized the shifting landscape of PCI being increasingly favored over surgery, particularly in treating left main (LM) shaft disease. Significant contributions by Seung-Jung Park, MD (Asan Medical Center, Seoul, Korea) were highlighted in this paradigm shift.
Previously, interventionists would often opt for surgery when confronted with challenging cases. However, King noted a trend toward choosing PCI, citing highly sophisticated PCI skills as a driving factor.
An illustrative case discussed was that of an 85-year-old male patient with a history of acute coronary syndrome (ACS), recurrent chest pain, and heart failure (Figure 1). The patient presented with multiple risk factors including diabetes, chronic renal failure, cerebrovascular accident, peripheral artery disease, and severe chronic obstructive pulmonary disease. The electrocardiogram confirmed LM disease consistent with ACS.
Initial coronary angiography revealed LM plus triple-vessel disease with complex lesions, including LM trifurcation disease and heavily calcified, diffuse long left anterior descending artery disease, alongside total occlusion of the proximal right coronary artery.
Given the patient's profile, both coronary artery bypass surgery (CABG) and PCI were considered. However, CABG was deemed prohibitive due to technical challenges, and the patient's advanced age and comorbidities. PCI posed its own difficulties, including the complexity of LM trifurcation lesions, the need for debulking procedures such as rotablation, and potential requirement for mechanical circulatory support. Assessing the postoperative outcomes, surgical mortality rates were projected to be high, prompting a thorough evaluation of the risks associated with both procedures. Ultimately, PCI was chosen for this high-risk patient, with successful completion reported.
King highlighted the lack of randomized controlled trials focusing on PCI for such complex cases. Instead, he referenced a recent registry study involving over 700 patients who were turned down for surgery and underwent PCI at specialized centers. The study showed that there was no difference in the actual mortality rate compared to the mortality rate predicted by the Society of Thoracic Surgeons score and EuroScore II, and that the symptoms of the patients improved 6 months after PCI compared to the baseline condition (Figure 2).
Looking ahead, King emphasized the need for further research to validate these findings and address key questions surrounding the selection of treatment modalities for complex cases. He advocated the establishment of local registries for high-risk patients to inform clinical decision-making.
In concluding the lecture, King left a lasting message for interventional cardiologists that no spectacular success will go unpunished and the more tough cases you take, the more you will get, which may be a good thing.
As the field continues to evolve, the quest for optimal treatment strategies for the most complex patients remains ongoing.
Live Case & Lecture 6: Complex PCI
Friday, April 26, 3:30 PM ~ 5:00 PM
Main Arena, Level 2
Edited by

Sang-Cheol Cho , MD
Yeosu Jeil Hospital, Korea (Republic of)

Leave a comment