News | TCTAP 2024
Long-term DOAC Management of AF and Stable CAD: Expectation on the EPIC-CAD Trial After the AFIRE Trial
All About New Data of Antithrombotics

Gi-Byoung Nam
Asan Medical Center, Republic of Korea
Atrial fibrillation (AF) concurrent with coronary artery disease (CAD) presents as a common clinical scenario. Approximately 30% of AF patients are reported to have CAD, with around half of them requiring percutaneous coronary intervention (PCI) during their lifetime. Conversely, 5-8% of patients undergoing PCI have concurrent AF, necessitating oral anticoagulation (OAC). Managing antithrombotic therapy in AF patients undergoing PCI is complex, as anticoagulation is crucial for preventing AF-related embolic stroke, while antiplatelet therapy is essential for preventing stent thrombosis (ST).
Finding a balance between ischemia prevention and bleeding risk is particularly challenging during the dynamic and unstable early post-PCI period. Traditionally, triple therapy (TT) of OAC plus dual antiplatelet therapy (DAPT) has been employed in recent decades. However, serious bleeding remains a significant obstacle with this approach. With the introduction of novel oral anticoagulants (NOACs) and subsequent large randomized clinical trials (RCTs), the duration of TT has been significantly reduced, typically confined to the hospital admission period. Extended TT (up to 1 month post-discharge) is recommended only in patients with high ischemic burden and low bleeding risk.
Antithrombotic management >6-12 months after PCI remains poorly understood. The incidence of ST is the highest (0.1-2.5%) in the first 30 days post-PCI and decreases over time (0.1-0.8%/year between 1-2 years). As bleeding risk remains high throughout the post-PCI period, and bleeding risk from combined anticoagulation and antiplatelet therapy is hierarchical, omitting antiplatelet agents 6-12 months after PCI has been proposed. Despite their plausibility, these recommendations lack validation from studies.
Recently, during 2018 and 2019, only two RCTs have been published. Optimizing Antithrombotic Care in Patients With Atrial Fibrillation and Coronary Stent (OAC-ALONE) trial was a prospective, multicenter, randomized, open-label, noninferiority trial comparing OAC alone with combined OAC and single antiplatelet therapy in patients with concurrent AF and stable CAD who had received coronary stents more than 1 year ago. The study was terminated prematurely due to slow patient enrollment, rendering it underpowered and inconclusive.
Atrial Fibrillation and Ischemic Events with Rivaroxaban in Patients with Stable Coronary Artery Disease (AFIRE) trial aimed to investigate whether rivaroxaban monotherapy is noninferior to combination therapy of rivaroxaban plus an antiplatelet agent in patients with AF and stable CAD who had revascularization more than 1 year ago, or those with angiographically confirmed CAD not requiring revascularization. The trial was discontinued early due to increased mortality in the combination therapy group. Rivaroxaban monotherapy was found to be noninferior for efficacy and superior for safety in patients with AF and stable CAD.
Based on these trials, current guidelines recommend NOACs only for long-term anticoagulation in patients with AF and CAD. Meanwhile, for patients who require long-term anticoagulation treatment, research is still limited on the appropriate duration of combined antiplatelet therapy that can minimize the long-term risk of bleeding while also reducing ischemic events, such as ST.
To provide further evidence on this issue, Gi-Byoung Nam, MD, and his team initiated the Edoxaban vs Edoxaban With antiPlatelet Agent In Patients With AF And Chronic Stable CAD (EPIC-CAD) trial to explore optimal antithrombotic therapy in patients with stable CAD and high-risk AF (Figure 1). The results of the EPIC-CAD trial are anticipated to provide additional insights into long-term antithrombotic management in these patients.
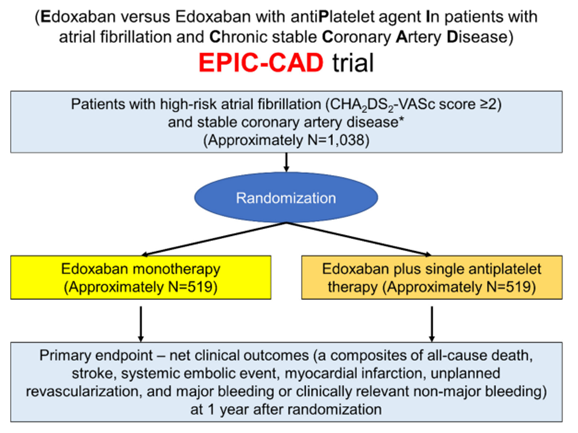
Figure 1. Main flow of the EPIC-CAD Trial
Hot Topics
All About New Data of Antithrombotics
Friday, April 26, 4:40 PM ~ 6:06 PM
Presentation Room 1, Level 1
Edited by

Osung Kwon, MD
The Catholic University of Korea Eunpyeong St. Mary's Hospital, Korea (Republic of)

Gi-Byoung Nam
Asan Medical Center, Republic of Korea
Atrial fibrillation (AF) concurrent with coronary artery disease (CAD) presents as a common clinical scenario. Approximately 30% of AF patients are reported to have CAD, with around half of them requiring percutaneous coronary intervention (PCI) during their lifetime. Conversely, 5-8% of patients undergoing PCI have concurrent AF, necessitating oral anticoagulation (OAC). Managing antithrombotic therapy in AF patients undergoing PCI is complex, as anticoagulation is crucial for preventing AF-related embolic stroke, while antiplatelet therapy is essential for preventing stent thrombosis (ST).
Finding a balance between ischemia prevention and bleeding risk is particularly challenging during the dynamic and unstable early post-PCI period. Traditionally, triple therapy (TT) of OAC plus dual antiplatelet therapy (DAPT) has been employed in recent decades. However, serious bleeding remains a significant obstacle with this approach. With the introduction of novel oral anticoagulants (NOACs) and subsequent large randomized clinical trials (RCTs), the duration of TT has been significantly reduced, typically confined to the hospital admission period. Extended TT (up to 1 month post-discharge) is recommended only in patients with high ischemic burden and low bleeding risk.
Antithrombotic management >6-12 months after PCI remains poorly understood. The incidence of ST is the highest (0.1-2.5%) in the first 30 days post-PCI and decreases over time (0.1-0.8%/year between 1-2 years). As bleeding risk remains high throughout the post-PCI period, and bleeding risk from combined anticoagulation and antiplatelet therapy is hierarchical, omitting antiplatelet agents 6-12 months after PCI has been proposed. Despite their plausibility, these recommendations lack validation from studies.
Recently, during 2018 and 2019, only two RCTs have been published. Optimizing Antithrombotic Care in Patients With Atrial Fibrillation and Coronary Stent (OAC-ALONE) trial was a prospective, multicenter, randomized, open-label, noninferiority trial comparing OAC alone with combined OAC and single antiplatelet therapy in patients with concurrent AF and stable CAD who had received coronary stents more than 1 year ago. The study was terminated prematurely due to slow patient enrollment, rendering it underpowered and inconclusive.
Atrial Fibrillation and Ischemic Events with Rivaroxaban in Patients with Stable Coronary Artery Disease (AFIRE) trial aimed to investigate whether rivaroxaban monotherapy is noninferior to combination therapy of rivaroxaban plus an antiplatelet agent in patients with AF and stable CAD who had revascularization more than 1 year ago, or those with angiographically confirmed CAD not requiring revascularization. The trial was discontinued early due to increased mortality in the combination therapy group. Rivaroxaban monotherapy was found to be noninferior for efficacy and superior for safety in patients with AF and stable CAD.
Based on these trials, current guidelines recommend NOACs only for long-term anticoagulation in patients with AF and CAD. Meanwhile, for patients who require long-term anticoagulation treatment, research is still limited on the appropriate duration of combined antiplatelet therapy that can minimize the long-term risk of bleeding while also reducing ischemic events, such as ST.
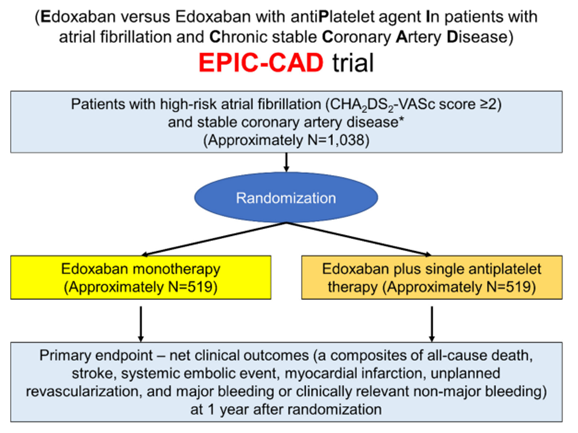
To provide further evidence on this issue, Gi-Byoung Nam, MD, and his team initiated the Edoxaban vs Edoxaban With antiPlatelet Agent In Patients With AF And Chronic Stable CAD (EPIC-CAD) trial to explore optimal antithrombotic therapy in patients with stable CAD and high-risk AF (Figure 1). The results of the EPIC-CAD trial are anticipated to provide additional insights into long-term antithrombotic management in these patients.
Hot Topics
All About New Data of Antithrombotics
Friday, April 26, 4:40 PM ~ 6:06 PM
Presentation Room 1, Level 1
Edited by

Osung Kwon, MD
The Catholic University of Korea Eunpyeong St. Mary's Hospital, Korea (Republic of)

Leave a comment