News | SEOUL VALVES 2021 Virtual
Data Hints at TAVR Expansion Into Low-risk Bicuspid AS but RCTs on Risky Morphology Still Missing
[AP VALVES & SH 2021] Cardiologists call for randomized trials defining morphology for positive TAVR outcomes in low surgical risk patients with bicuspid aortic stenosis
Heart teams around the world are calling for precise randomized data on transcatheter aortic valve replacement (TAVR) for bicuspid aortic valves (BAV)-aortic stenosis (AS) patients at low surgical risk.
 Raj R. Makkar, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, USA) presented a synopsis of limited but existing TAVR data and sketched the way forward on the understudied and largely RCT-excluded patient group at AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) on August 6.
Raj R. Makkar, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, USA) presented a synopsis of limited but existing TAVR data and sketched the way forward on the understudied and largely RCT-excluded patient group at AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) on August 6.
Current data shows TAVR has great potential benefits for low-risk bicuspid AS patients but is being used only "selectively" in the patient group. The lack of concrete evidence for bicuspid AS has ruled out the transcatheter procedure for many patients.
"Investigational Device Exemption (IDE) trial data have helped label expansion for TAVR in the past decade, but anatomically heterogeneous bicuspid AS patients with frequent aortopathy - not found in previous IDEs - are becoming more common," Makkar said.
Although researchers published favorable study results with both Sapien (Edwards Lifesciences) and Evolut (Medtronic) systems in real-life and registry studies, much-needed RCT data are still missing.
It's more than just the eligibility of the first TAVR procedure; it's about how patients will live for the next 8 to 10 years.
In the absence of RCT data, heart teams can use existing data and cardiac computer tomography (CT) phenotyping to plan the procedure and minimize risk, especially for patients who are still very much contraindicated for the TAVR procedure, Makkar said.
"While bicuspid TAVR is justifiable irrespective of surgical risk, high-risk anatomical features such as extreme calcium, heavy-calcified raphe, and concomitant aortopathy should prompt consideration for surgical AVR in low-risk patients," he said. "We need further randomized trials and prospective registries - especially in patients with lower surgical risk - to guide treatment."
TAVR indications expand rapidly as surgery replacement, but BAV data not enough
Although TAVR was a novel stenting procedure as little as two decades ago, a series of successful RCTs published over the past 15 years has rapidly expanded its indications to various patient groups.
Despite favorable data, these RCTs excluded BAV patients due to safety issues.
TAVR is justifiable irrespective of surgical risk, but high-risk anatomical features should prompt consideration for SAVR in low-risk patients.
BAV is one of the most common hereditary heart valve diseases wherein the aortic valve has only two cusps instead of three and occurs in about 1-2% of the total population. The condition increases risk of aortic stenosis - a condition when the heart's valve doesn't open properly, leading the reduced or blocked blood flow from the heart to the aorta and body.
Treatment for severe BAV may require open-heart surgery (SAVR) to repair or replace the aortic valve. Statistics show nearly 25% of patients over 80 years of age were referred for aortic valve replacement (AVR).12
As opposed to SAVR, the minimally invasive TAVR procedure has become an increasingly popular treatment option for both the elderly and younger populations.
"We are going to encounter bicuspid AS with greater frequency as TAVR expands into younger patient groups," Makkar said. "Currently, up to 50% of young patients receiving surgical aortic valve replacement (SAVR) have bicuspid valves."
"Surgical outcomes in young bicuspid AS patients are excellent, making it reasonable to expect robust evidence for TAVR to replace SAVR for these patients," he added.
The U.S. Food and Drug Administration (FDA) and European health regulators had approved TAVR for low surgical risk patients regardless of aortic valve anatomy in August and November 2019, respectively - thereby expanding TAVR indications beyond intermediate or higher SAVR risk groups.34
However, most international guidelines still take a conservative stance by recommending SAVR - not TAVR - for BAV patients.
Cardiologists are now calling for robust data to resolve the treatment ambiguity of the heterogeneous BAV group as they face an increasing number of them in clinical practice.
We absolutely need randomized trials and prospective registries to guide treatment for low-risk patients.
At AP VALVES & SH 2021, Makkar presented study findings by his research team that examined the difference in mortality and stroke between bicuspid and tricuspid AS patients undergoing TAVR in a registry-based cohort study in 2019 published in the Journal of the American Medical Association (JAMA).5
Researchers ran a propensity-matched analysis on the U.S. Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapies (STS/ACC TVT) Registry, including more than 2,700 pairs of bicuspid and tricuspid AS patients (average age: 74; mean STS score: 4.9%).
Results showed that TAVR outcomes between bicuspid and tricuspid patients did not differ regarding mortality (30-day mortality: 2.6% vs. 2.5%; HR, 1.04. 95% CI, 0.74-1.47).
30-day stroke rates were higher in bicuspid (2.5% vs. 1.6%; 0.88-0.9%). Implantation of new pacemakers was also "slightly but significantly higher" in bicuspid (9.1% vs. 7.5%, HR 1.23, 1.02-1.49).
1-year mortality rates (10.5% vs 12.0%; HR, 0.90, 0.73-1.10, p=0.31) and 1-year stroke rates (3.4% vs 3.1%; HR, 1.28, 0.91-1.79, p=0.16) were also favorable, indicating no difference between bicuspid and tricuspid.
"Procedural outcomes were good in this classic study. The rate of conversion to open surgery for bicuspid AS was 0.9%, which is low but still higher than tricuspid AS," Makkar said. "Annulus rupture (0.3%), aortic dissection (0.3%), and coronary obstruction (0.4%) were all less than 1%."
Although researchers ran the analysis with the balloon-expandable Sapien 3 platform, the STS/ACC TVT Registry also compiled similar data on the Evolut R and Evolut PRO valves, he added.
'Excellent' TAVR outcomes after US approval for low-risk groups signal potential
Makkar and Sung-han Yoon, MD (Cedars Sinai Medical Center, Los Angeles, USA) also investigated TAVR outcomes in the low-risk patient group after FDA approval for low surgical risk groups in 2019.6
The study7 examined outcomes of nearly 37,000 low-risk bicuspid or tricuspid AS patients who underwent TAVR with Sapien 3 or Sapien 3 Ultra from the STS/ACC TVT Registry from June 2015 to October 2020. Propensity-matching produced 3,168 pairs of bicuspid and tricuspid AS patients. (average age: 68.8; mean STS score: 1.7%)
Researchers examined death and stroke incidence as the primary endpoint. Secondary endpoints included procedural complications, echocardiogram outcomes, and functional status outcomes.
Findings presented at EURO PCR 2021 and simultaneously published in JAMA showed 30-day outcomes were similar (bicuspid vs. tricuspid AS):
- Conversion to open heart surgery: 0.4% vs. 0.4%, p=0.85
- Annulus rupture: 0.2% vs. 0.1%, p=1.00
- Aortic dissection: 0.1% vs. 0%, p=0.5
- Coronary obstruction: 0.3% vs. 0.1%, p=0.37
- Need for second valve 0.3% vs. 0.1%, p=0.11
- All-cause mortality: 0.9% vs. 0.8%, p=0.55
- All-stroke: 1.4% vs. 1.2%, p=0.55
- In-hospital all-cause mortality: 0.6% vs. 0.4%, p=NS
"These are excellent outcomes when compared to tricuspid AS, or even the contemporary surgical series in bicuspid AS," Makkar said. "Conversion to open-heart surgery occurred 1.4% of the time for bicuspid, and this was the same for tricuspid. 30-day mortality was less than 1%, and stroke rates were similar as well."
"Even 1-year rates showed no difference," he continued. "If anything, bicuspid AS had lower mortality than tricuspid, and this almost reached statistical significance. This data on nearly 7,000 patients reassures the heart team that bicuspid outcomes are not worse than tricuspid."
1-year mortality and stroke outcomes followed the favorable trend (bicuspid vs. tricuspid AS):
- 1-year mortality: 8.6% vs. 9.8% (HR 0.90, 0.78-1.04, p=0.157)
- 1-year stroke: 2.8% vs. 3.1% (HR 0.96, 0.78-1.20, p=0.748)
New pacemaker implantation and aortic valve intervention (1.16% vs. 0.4%) rates were higher for bicuspid AS but showed a minimal difference. NYHA and KCCQ scores also improved significantly in both groups, while aortic valve gradient and valve areas were similar.
'Valve morphology plays critical role in TAVR outcomes'
In a detailed analysis, Abhjeet Dhoble, MD (University of Texas Health Science Center, Houston, USA), Yoon, and colleagues found that specific BAV morphology such as raphe calcification and leaflet calcification was associated with poorer clinical outcomes8.
A quarter of patients presented a combo of calcified raphe and excess leaflet calcium - and that meant more aortic injury.
Researchers enrolled 1,034 patients with CT-confirmed bicuspid anatomy from eight countries (Denmark, France, Germany, Israel, Italy, the Netherlands, Switzerland, and the U.S.) and classified them as either type-0 BAV (10.3%); type-1 non-calcified raphe (45.1%); or type-1 calcified raphe 44.6%.
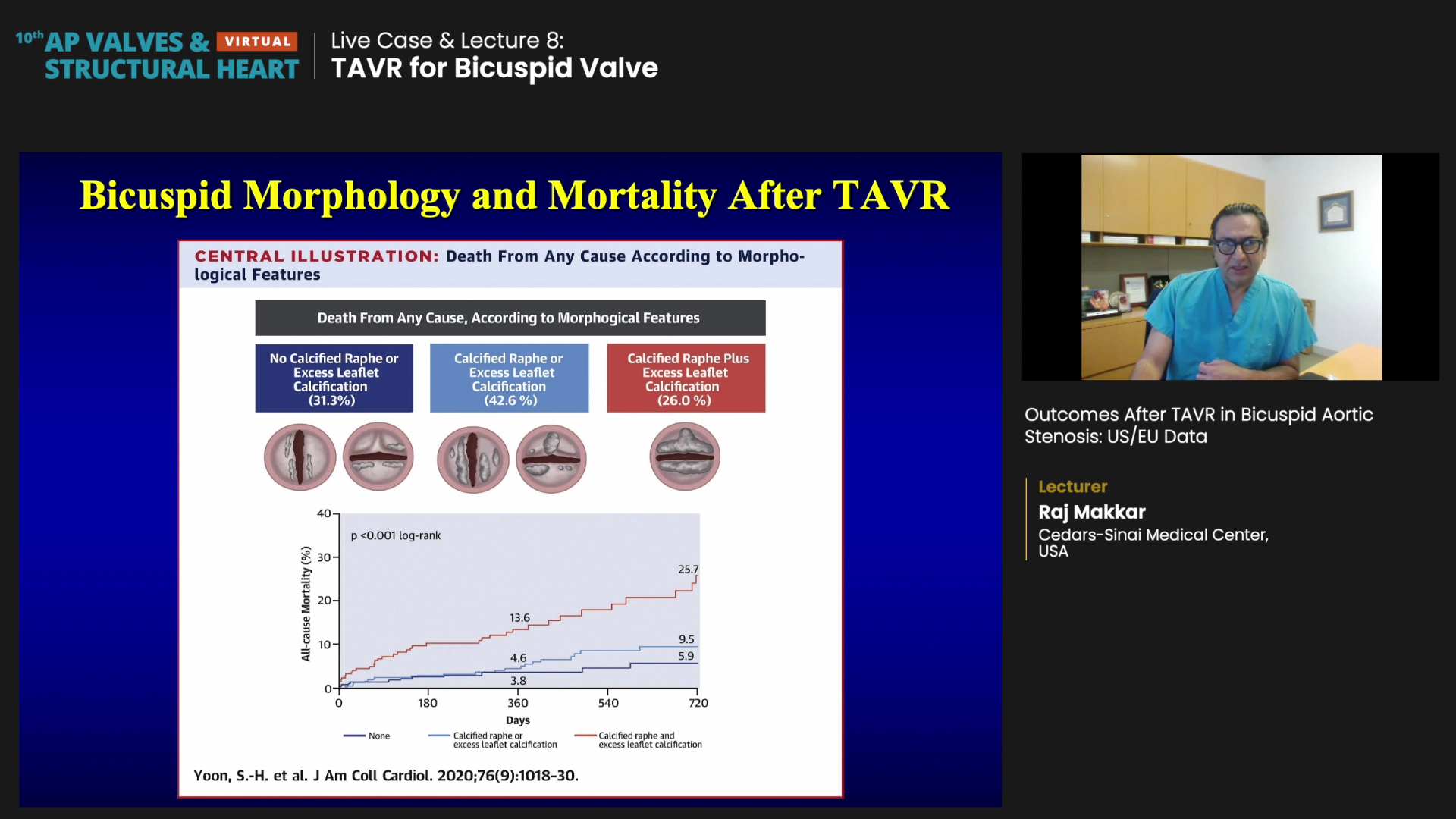
Patients underwent TAVR with either Sapien 3 (71.6%) or Evolut R/PRO (18.2%). The mean age was 74.7 years; the mean STS score was 3.7%; transfemoral TAVR accounted for 94.3%.
Stroke and mortality results showed:
- 30-day stroke: 2.4%
- 30-day mortality: 2%
- 1-year mortality: 6.7%
- 2-year mortality: 12.5%
Strikingly, multivariate analysis showed 26% of enrolled patients had calcified raphe and excess leaflet calcification and had a significantly higher 2-year all-cause mortality than patients with one or none of these morphological features (25.7% vs. 9.5% vs. 5.9%, log-rank p < 0.001).9
Furthermore, patients with both morphological features had higher rates of aortic root injury (p<0.001); moderate-to-severe paravalvular regurgitation (p=0.002), and 30-day mortality (p=0.016).
"A quarter of patients presented a combination of calcified raphe and excess leaflet calcium and results showed the combination of calcified raphe and excess leaflet calcium translated to more aortic injury," Makkar said.
Considering that valve morphology in bicuspid AS plays a critical role, 4D CT imaging can help identify phenotypes and rule-in or rule-out patients for the TAVR procedure as an interim solution, he added.
"We need to consider the patient's lifetime management when deciding between TAVR and SAVR for younger people who may require multiple procedures down the road, meaning we need RCT data. It's not just the eligibility of the first TAVR procedure; it's about how patients will live for the next 8 to 10 years."
- https://eymj.org/DOIx.php?id=10.3349/ymj.2019.60.9.816
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.048048
- https://www.fda.gov/news-events/press-announcements/fda-expands-indication-several-transcatheter-heart-valves-patients-low-risk-death-or-major
- https://www.tctmd.com/news/sapien-3-valve-approved-europe-low-risk-patients
- https://jamanetwork.com/journals/jama/fullarticle/2735503
- https://www.tctmd.com/news/fda-expands-tavr-indication-low-risk-patients
- https://www.tctmd.com/news/good-tavi-results-seen-bicuspid-aortic-stenosis-tvt-registry
- https://www.jacc.org/doi/abs/10.1016/j.jacc.2020.07.005?_ga=2.170753056.1656457118.1628054161-1121651248.1628054161
- https://www.acc.org/latest-in-cardiology/journal-scans/2020/08/24/14/02/bicuspid-aortic-valve-morphology-and-outcomes
Edited by

Do-Yoon Kang, MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read Biography
Heart teams around the world are calling for precise randomized data on transcatheter aortic valve replacement (TAVR) for bicuspid aortic valves (BAV)-aortic stenosis (AS) patients at low surgical risk.
 Raj R. Makkar, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, USA) presented a synopsis of limited but existing TAVR data and sketched the way forward on the understudied and largely RCT-excluded patient group at AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) on August 6.
Raj R. Makkar, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, USA) presented a synopsis of limited but existing TAVR data and sketched the way forward on the understudied and largely RCT-excluded patient group at AP Valves & Structural Heart Virtual (AP VALVES & SH 2021) on August 6.
Current data shows TAVR has great potential benefits for low-risk bicuspid AS patients but is being used only "selectively" in the patient group. The lack of concrete evidence for bicuspid AS has ruled out the transcatheter procedure for many patients.
"Investigational Device Exemption (IDE) trial data have helped label expansion for TAVR in the past decade, but anatomically heterogeneous bicuspid AS patients with frequent aortopathy - not found in previous IDEs - are becoming more common," Makkar said.
Although researchers published favorable study results with both Sapien (Edwards Lifesciences) and Evolut (Medtronic) systems in real-life and registry studies, much-needed RCT data are still missing.
It's more than just the eligibility of the first TAVR procedure; it's about how patients will live for the next 8 to 10 years.
In the absence of RCT data, heart teams can use existing data and cardiac computer tomography (CT) phenotyping to plan the procedure and minimize risk, especially for patients who are still very much contraindicated for the TAVR procedure, Makkar said.
"While bicuspid TAVR is justifiable irrespective of surgical risk, high-risk anatomical features such as extreme calcium, heavy-calcified raphe, and concomitant aortopathy should prompt consideration for surgical AVR in low-risk patients," he said. "We need further randomized trials and prospective registries - especially in patients with lower surgical risk - to guide treatment."
TAVR indications expand rapidly as surgery replacement, but BAV data not enough
Although TAVR was a novel stenting procedure as little as two decades ago, a series of successful RCTs published over the past 15 years has rapidly expanded its indications to various patient groups.
Despite favorable data, these RCTs excluded BAV patients due to safety issues.
TAVR is justifiable irrespective of surgical risk, but high-risk anatomical features should prompt consideration for SAVR in low-risk patients.
BAV is one of the most common hereditary heart valve diseases wherein the aortic valve has only two cusps instead of three and occurs in about 1-2% of the total population. The condition increases risk of aortic stenosis - a condition when the heart's valve doesn't open properly, leading the reduced or blocked blood flow from the heart to the aorta and body.
Treatment for severe BAV may require open-heart surgery (SAVR) to repair or replace the aortic valve. Statistics show nearly 25% of patients over 80 years of age were referred for aortic valve replacement (AVR).12
As opposed to SAVR, the minimally invasive TAVR procedure has become an increasingly popular treatment option for both the elderly and younger populations.
"We are going to encounter bicuspid AS with greater frequency as TAVR expands into younger patient groups," Makkar said. "Currently, up to 50% of young patients receiving surgical aortic valve replacement (SAVR) have bicuspid valves."
"Surgical outcomes in young bicuspid AS patients are excellent, making it reasonable to expect robust evidence for TAVR to replace SAVR for these patients," he added.
The U.S. Food and Drug Administration (FDA) and European health regulators had approved TAVR for low surgical risk patients regardless of aortic valve anatomy in August and November 2019, respectively - thereby expanding TAVR indications beyond intermediate or higher SAVR risk groups.34
However, most international guidelines still take a conservative stance by recommending SAVR - not TAVR - for BAV patients.
Cardiologists are now calling for robust data to resolve the treatment ambiguity of the heterogeneous BAV group as they face an increasing number of them in clinical practice.
We absolutely need randomized trials and prospective registries to guide treatment for low-risk patients.
At AP VALVES & SH 2021, Makkar presented study findings by his research team that examined the difference in mortality and stroke between bicuspid and tricuspid AS patients undergoing TAVR in a registry-based cohort study in 2019 published in the Journal of the American Medical Association (JAMA).5
Researchers ran a propensity-matched analysis on the U.S. Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapies (STS/ACC TVT) Registry, including more than 2,700 pairs of bicuspid and tricuspid AS patients (average age: 74; mean STS score: 4.9%).
Results showed that TAVR outcomes between bicuspid and tricuspid patients did not differ regarding mortality (30-day mortality: 2.6% vs. 2.5%; HR, 1.04. 95% CI, 0.74-1.47).
30-day stroke rates were higher in bicuspid (2.5% vs. 1.6%; 0.88-0.9%). Implantation of new pacemakers was also "slightly but significantly higher" in bicuspid (9.1% vs. 7.5%, HR 1.23, 1.02-1.49).
1-year mortality rates (10.5% vs 12.0%; HR, 0.90, 0.73-1.10, p=0.31) and 1-year stroke rates (3.4% vs 3.1%; HR, 1.28, 0.91-1.79, p=0.16) were also favorable, indicating no difference between bicuspid and tricuspid.
"Procedural outcomes were good in this classic study. The rate of conversion to open surgery for bicuspid AS was 0.9%, which is low but still higher than tricuspid AS," Makkar said. "Annulus rupture (0.3%), aortic dissection (0.3%), and coronary obstruction (0.4%) were all less than 1%."
Although researchers ran the analysis with the balloon-expandable Sapien 3 platform, the STS/ACC TVT Registry also compiled similar data on the Evolut R and Evolut PRO valves, he added.
'Excellent' TAVR outcomes after US approval for low-risk groups signal potential
Makkar and Sung-han Yoon, MD (Cedars Sinai Medical Center, Los Angeles, USA) also investigated TAVR outcomes in the low-risk patient group after FDA approval for low surgical risk groups in 2019.6
The study7 examined outcomes of nearly 37,000 low-risk bicuspid or tricuspid AS patients who underwent TAVR with Sapien 3 or Sapien 3 Ultra from the STS/ACC TVT Registry from June 2015 to October 2020. Propensity-matching produced 3,168 pairs of bicuspid and tricuspid AS patients. (average age: 68.8; mean STS score: 1.7%)
Researchers examined death and stroke incidence as the primary endpoint. Secondary endpoints included procedural complications, echocardiogram outcomes, and functional status outcomes.
Findings presented at EURO PCR 2021 and simultaneously published in JAMA showed 30-day outcomes were similar (bicuspid vs. tricuspid AS):
- Conversion to open heart surgery: 0.4% vs. 0.4%, p=0.85
- Annulus rupture: 0.2% vs. 0.1%, p=1.00
- Aortic dissection: 0.1% vs. 0%, p=0.5
- Coronary obstruction: 0.3% vs. 0.1%, p=0.37
- Need for second valve 0.3% vs. 0.1%, p=0.11
- All-cause mortality: 0.9% vs. 0.8%, p=0.55
- All-stroke: 1.4% vs. 1.2%, p=0.55
- In-hospital all-cause mortality: 0.6% vs. 0.4%, p=NS
"These are excellent outcomes when compared to tricuspid AS, or even the contemporary surgical series in bicuspid AS," Makkar said. "Conversion to open-heart surgery occurred 1.4% of the time for bicuspid, and this was the same for tricuspid. 30-day mortality was less than 1%, and stroke rates were similar as well."
"Even 1-year rates showed no difference," he continued. "If anything, bicuspid AS had lower mortality than tricuspid, and this almost reached statistical significance. This data on nearly 7,000 patients reassures the heart team that bicuspid outcomes are not worse than tricuspid."
1-year mortality and stroke outcomes followed the favorable trend (bicuspid vs. tricuspid AS):
- 1-year mortality: 8.6% vs. 9.8% (HR 0.90, 0.78-1.04, p=0.157)
- 1-year stroke: 2.8% vs. 3.1% (HR 0.96, 0.78-1.20, p=0.748)
New pacemaker implantation and aortic valve intervention (1.16% vs. 0.4%) rates were higher for bicuspid AS but showed a minimal difference. NYHA and KCCQ scores also improved significantly in both groups, while aortic valve gradient and valve areas were similar.
'Valve morphology plays critical role in TAVR outcomes'
In a detailed analysis, Abhjeet Dhoble, MD (University of Texas Health Science Center, Houston, USA), Yoon, and colleagues found that specific BAV morphology such as raphe calcification and leaflet calcification was associated with poorer clinical outcomes8.
A quarter of patients presented a combo of calcified raphe and excess leaflet calcium - and that meant more aortic injury.
Researchers enrolled 1,034 patients with CT-confirmed bicuspid anatomy from eight countries (Denmark, France, Germany, Israel, Italy, the Netherlands, Switzerland, and the U.S.) and classified them as either type-0 BAV (10.3%); type-1 non-calcified raphe (45.1%); or type-1 calcified raphe 44.6%.
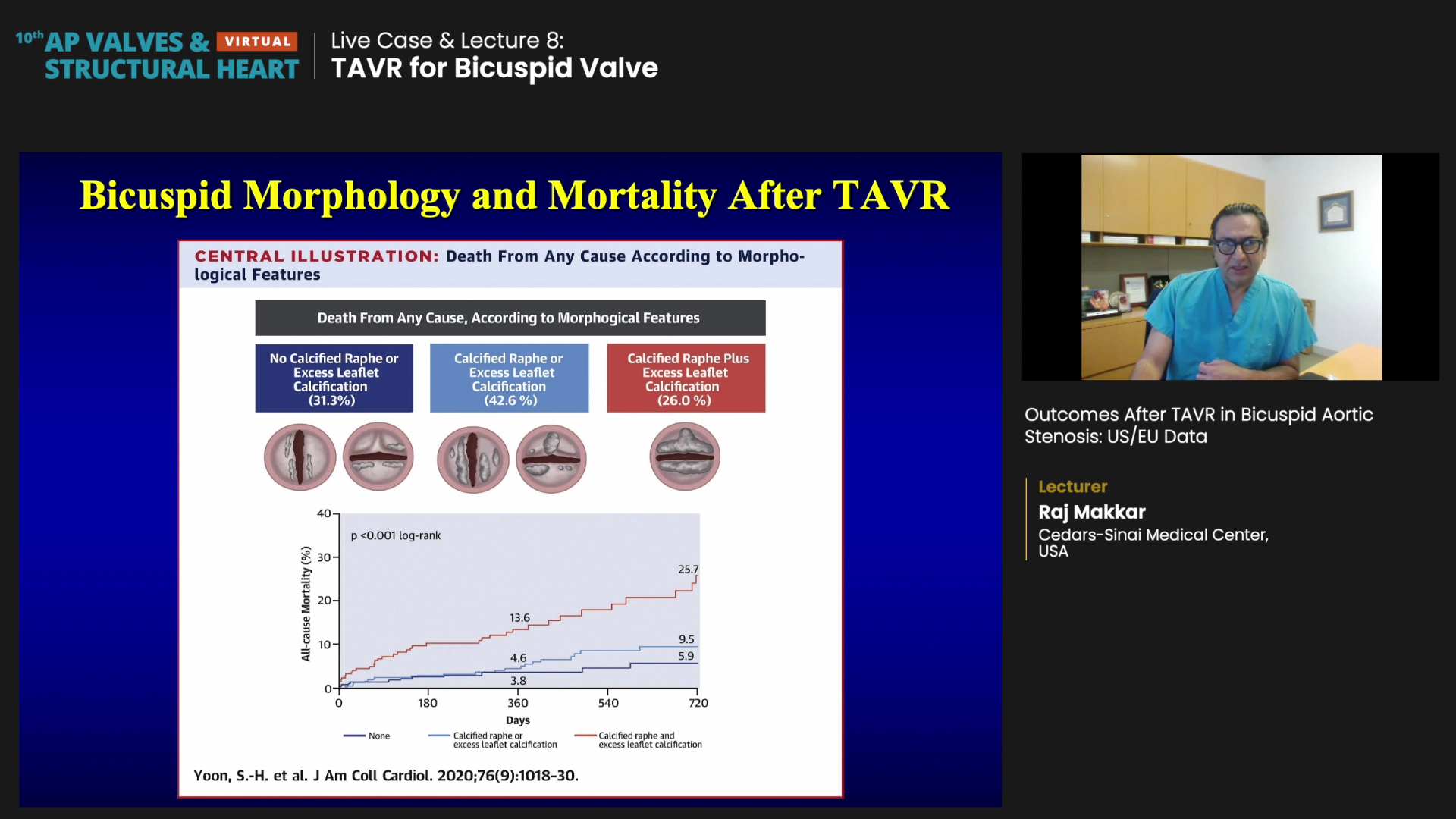
Patients underwent TAVR with either Sapien 3 (71.6%) or Evolut R/PRO (18.2%). The mean age was 74.7 years; the mean STS score was 3.7%; transfemoral TAVR accounted for 94.3%.
Stroke and mortality results showed:
- 30-day stroke: 2.4%
- 30-day mortality: 2%
- 1-year mortality: 6.7%
- 2-year mortality: 12.5%
Strikingly, multivariate analysis showed 26% of enrolled patients had calcified raphe and excess leaflet calcification and had a significantly higher 2-year all-cause mortality than patients with one or none of these morphological features (25.7% vs. 9.5% vs. 5.9%, log-rank p < 0.001).9
Furthermore, patients with both morphological features had higher rates of aortic root injury (p<0.001); moderate-to-severe paravalvular regurgitation (p=0.002), and 30-day mortality (p=0.016).
"A quarter of patients presented a combination of calcified raphe and excess leaflet calcium and results showed the combination of calcified raphe and excess leaflet calcium translated to more aortic injury," Makkar said.
Considering that valve morphology in bicuspid AS plays a critical role, 4D CT imaging can help identify phenotypes and rule-in or rule-out patients for the TAVR procedure as an interim solution, he added.
"We need to consider the patient's lifetime management when deciding between TAVR and SAVR for younger people who may require multiple procedures down the road, meaning we need RCT data. It's not just the eligibility of the first TAVR procedure; it's about how patients will live for the next 8 to 10 years."
- https://eymj.org/DOIx.php?id=10.3349/ymj.2019.60.9.816
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.048048
- https://www.fda.gov/news-events/press-announcements/fda-expands-indication-several-transcatheter-heart-valves-patients-low-risk-death-or-major
- https://www.tctmd.com/news/sapien-3-valve-approved-europe-low-risk-patients
- https://jamanetwork.com/journals/jama/fullarticle/2735503
- https://www.tctmd.com/news/fda-expands-tavr-indication-low-risk-patients
- https://www.tctmd.com/news/good-tavi-results-seen-bicuspid-aortic-stenosis-tvt-registry
- https://www.jacc.org/doi/abs/10.1016/j.jacc.2020.07.005?_ga=2.170753056.1656457118.1628054161-1121651248.1628054161
- https://www.acc.org/latest-in-cardiology/journal-scans/2020/08/24/14/02/bicuspid-aortic-valve-morphology-and-outcomes
Edited by

Do-Yoon Kang, MD
Asan Medical Center, Korea (Republic of)
Written by



Leave a comment