News | TCTAP 2022
'ISCHEMIA findings bolster argument for invasive revascularization in stable CAD'
Gregg W. Stone, MD emphasizes revasc benefits with PCI, CABG for patients with stable ischemic heart disease at TCTAP 2022
Highlights
The nuanced but important findings of the ISCHEMIA trial may bump up invasive revascularization as an initial treatment strategy for patients with stable coronary artery disease (CAD).
 At the 27th TCTAP 2022 on Apr 28, Gregg W. Stone, MD (Mount Sinai Hospital/Cardiovascular Research Foundation, New York, USA) assessed ISCHEMIA findings to determine which stable CAD patients benefit from percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG).
At the 27th TCTAP 2022 on Apr 28, Gregg W. Stone, MD (Mount Sinai Hospital/Cardiovascular Research Foundation, New York, USA) assessed ISCHEMIA findings to determine which stable CAD patients benefit from percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG).
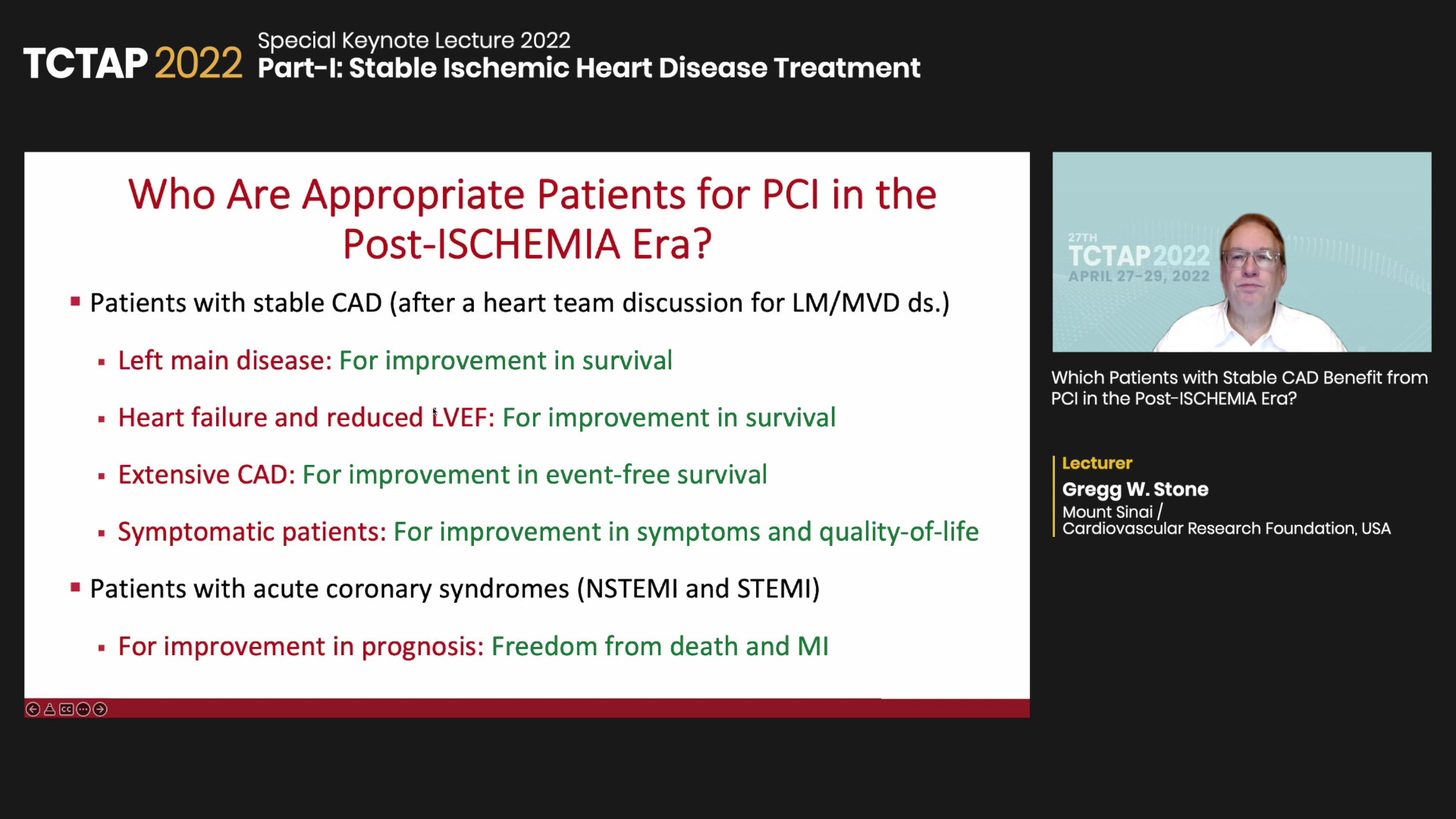
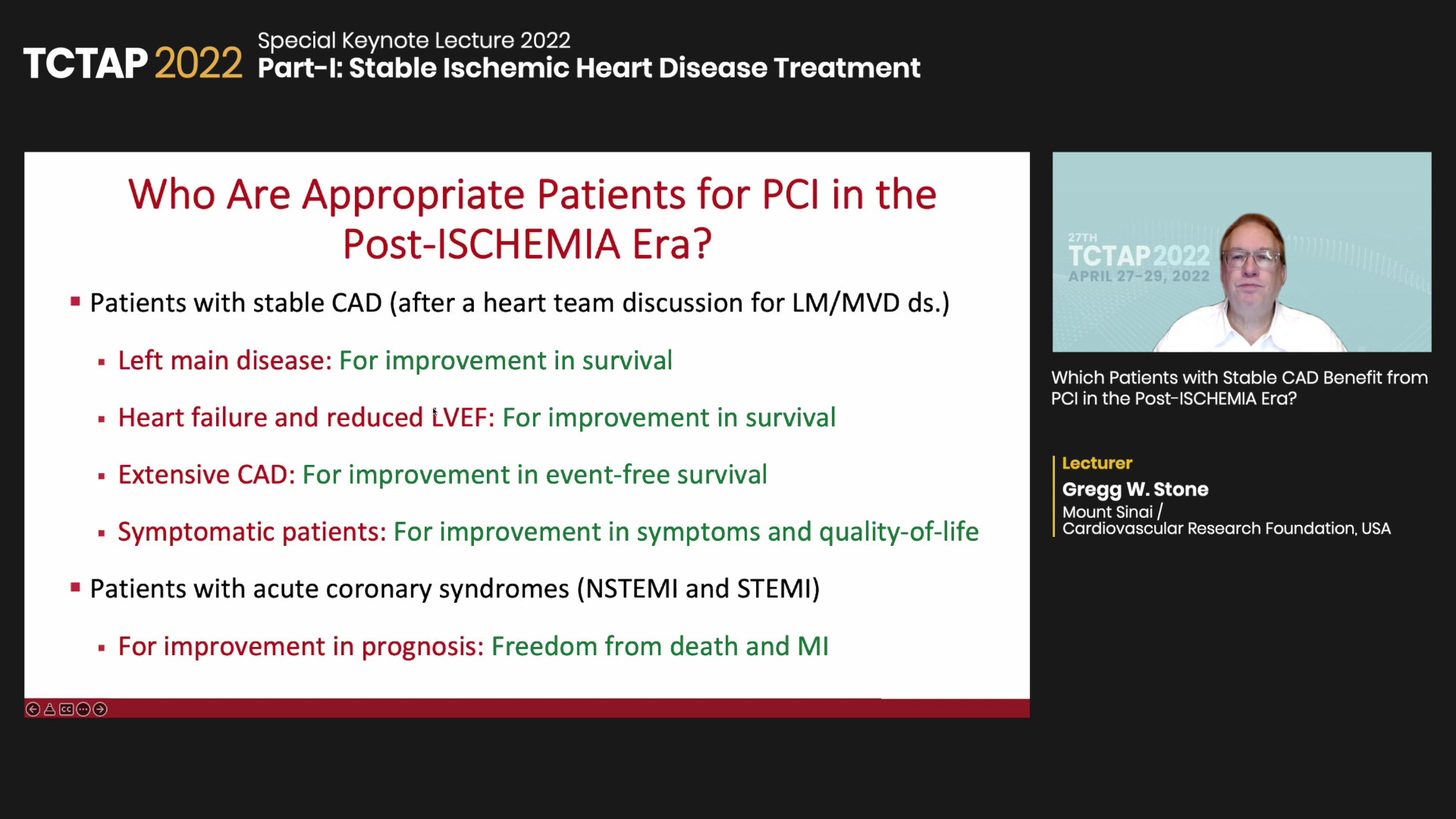
"An in-depth heart team discussion helps select an optimal procedure for patients with complex left main (LM) or multivessel disease," Stone said. "When PCI is a safe option, ISCHEMIA shows that many CAD patients, including LM, heart failure (HF), reduced left ventricular ejection fraction (LVEF), and extensive or symptomatic CAD can benefit from the procedure."
Stable CAD is a leading form of heart disease that presents asymptomatic or non-progressive symptoms. Treatment may involve traditional open-heart surgery with CABG or a minimally invasive stenting procedure with PCI.
Although PCI is an established treatment for acute coronary syndrome (ACS), the COURAGE and BARI 2D trials, among others, showed that PCI in stable CAD did not improve the primary composite outcome comprised of mortality, myocardial infarction (MI), and 5-year major adverse cardiovascular events (MACE) over guideline-directed medical therapy (GDMT) alone.
Current guidelines recommend GDMT as the first-line treatment for stable CAD and include lifestyle modifications with antiplatelet and lipid-lowering therapy. For stable CAD, PCI is recommended only for:
The randomized controlled ISCHEMIA trial, led by David J. Maron, MD (Stanford/Cedars-Sinai Medical Center, California, USA) and published in the New England Journal of Medicine (NEJM) in 2020, seemed to echo the sentiment.
The trial enrolled and randomized 5,179 patients with moderate or severe ischemia to receive initial invasive therapy plus medical therapy (angiography, revasc when feasible) or initial conservative treatment alone. The primary composite outcome was cardiovascular mortality, MI, hospitalization for unstable angina, HF, or resuscitated cardiac arrest.
Results over a median of 3.2 years showed that initial PCI or CABG did not reduce primary composite events more than conservative medical therapy alone (invasive arm 318 vs. conservative arm 352).
Investigators also noted that the invasive strategy arm had an initial higher 6-month cumulative event rate (5.3% vs. 3.4%, difference 1.9%p, 95% CI, 0.8-3.0), but the risk dropped below that of the conservative arm at 5 years (16.4% vs. 18.2%, diff -1.8%p, -4.7 to 1.0).
Although ISCHEMIA initially appeared to cement the argument for conservative therapy in stable CAD, closer examination showed the initial harm associated with invasive revascularization flipped over to a near statistically significant benefit at 5-years.
"There was an initial 2% harm with the invasive strategy (mean event-free time difference: 1.9%, HR 1.9%, 0.8-3.0%),” Stone said. “But the curves crossed over at about 2 years (-2.2%, -4.4-0.0%), and further indicated a borderline statistically significant 2.2% benefit with the invasive strategy (HR 0.93, 0.80-1.08, P=0.34)."
"There was no major difference in event-free survival, marked by the area between the curves," he added. “Investigators also found no significant difference for key pre-specified subgroups including age, sex, diabetes and even anatomic complexity.”
Post-hoc subgroup analysis using the modified Duke Prognostic Index also demonstrated a clear prognostic benefit with CABG and PCI for patients with triple-vessel CAD (≥70%) or double-vessel disease (≥70% including proximal LAD), Stone said.
A second subgroup analysis further showed significant prognostic improvement with PCI and CABG for patients with left ventricular dysfunction (EF 35-45%) or heart failure (NYHA Class I-II).
"As negative trials, these subgroup analyses remain only hypothesis-generating and require conservative assessment," Stone said. "But these results clearly show the prognostic benefits of invasive revascularization consistent with earlier CABG studies like STICH."
As for an optimal revascularization strategy, Stone emphasized weighing the pros and cons of each approach based on a recent meta-analysis published by Marc S. Sabatine, MD (Brigham Women's Hospital, Massachusetts, USA) and colleagues in the Lancet.
"Asking where to apply PCI asks what should be done in LM and multivessel disease," Stone said. "The recent meta-analysis that compared DES-PCI versus CABG in left main showed no significant difference in 5-year all-cause mortality but tradeoffs with each approach like CABG with lower mortality rates in high SYNTAX scores and lower 1-year stroke rates with PCI."
Regarding quality-of-life (QoL), two respective surveys on the SYNTAX and EXCEL trials showed similar long-term QoL outcomes between PCI and CABG, albeit a small early benefit with PCI stemming from reduced post-procedural physical limitations.
"PCI can improve survival for LM, HF, and reduced LVEF patients with stable CAD and extensive or symptomatic CAD," Stone said. “Importantly, primary PCI extends beyond stable CAD with benefits reported in ACS-STEMI for mortality, reinfarction, stroke or recurrent ischemia and NSTE-ACS for MI."
Edited by

Cheol Hyun Lee, MD
Keimyung University Dongsan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read Biography
Maron, David J., et al. “Initial Invasive or Conservative Strategy for Stable Coronary Disease.” New England Journal of Medicine, vol. 382, no. 15, 2020, pp. 1395-1407.
Stone disclosed grants from NHLBI; Mount Sinai Hospital receives research funding from Abbott.
The nuanced but important findings of the ISCHEMIA trial may bump up invasive revascularization as an initial treatment strategy for patients with stable coronary artery disease (CAD).
 At the 27th TCTAP 2022 on Apr 28, Gregg W. Stone, MD (Mount Sinai Hospital/Cardiovascular Research Foundation, New York, USA) assessed ISCHEMIA findings to determine which stable CAD patients benefit from percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG).
At the 27th TCTAP 2022 on Apr 28, Gregg W. Stone, MD (Mount Sinai Hospital/Cardiovascular Research Foundation, New York, USA) assessed ISCHEMIA findings to determine which stable CAD patients benefit from percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG).
"An in-depth heart team discussion helps select an optimal procedure for patients with complex left main (LM) or multivessel disease," Stone said. "When PCI is a safe option, ISCHEMIA shows that many CAD patients, including LM, heart failure (HF), reduced left ventricular ejection fraction (LVEF), and extensive or symptomatic CAD can benefit from the procedure."
Stable CAD is a leading form of heart disease that presents asymptomatic or non-progressive symptoms. Treatment may involve traditional open-heart surgery with CABG or a minimally invasive stenting procedure with PCI.
Although PCI is an established treatment for acute coronary syndrome (ACS), the COURAGE and BARI 2D trials, among others, showed that PCI in stable CAD did not improve the primary composite outcome comprised of mortality, myocardial infarction (MI), and 5-year major adverse cardiovascular events (MACE) over guideline-directed medical therapy (GDMT) alone.
Current guidelines recommend GDMT as the first-line treatment for stable CAD and include lifestyle modifications with antiplatelet and lipid-lowering therapy. For stable CAD, PCI is recommended only for:
The randomized controlled ISCHEMIA trial, led by David J. Maron, MD (Stanford/Cedars-Sinai Medical Center, California, USA) and published in the New England Journal of Medicine (NEJM) in 2020, seemed to echo the sentiment.
The trial enrolled and randomized 5,179 patients with moderate or severe ischemia to receive initial invasive therapy plus medical therapy (angiography, revasc when feasible) or initial conservative treatment alone. The primary composite outcome was cardiovascular mortality, MI, hospitalization for unstable angina, HF, or resuscitated cardiac arrest.
Results over a median of 3.2 years showed that initial PCI or CABG did not reduce primary composite events more than conservative medical therapy alone (invasive arm 318 vs. conservative arm 352).
Investigators also noted that the invasive strategy arm had an initial higher 6-month cumulative event rate (5.3% vs. 3.4%, difference 1.9%p, 95% CI, 0.8-3.0), but the risk dropped below that of the conservative arm at 5 years (16.4% vs. 18.2%, diff -1.8%p, -4.7 to 1.0).
Although ISCHEMIA initially appeared to cement the argument for conservative therapy in stable CAD, closer examination showed the initial harm associated with invasive revascularization flipped over to a near statistically significant benefit at 5-years.
"There was an initial 2% harm with the invasive strategy (mean event-free time difference: 1.9%, HR 1.9%, 0.8-3.0%),” Stone said. “But the curves crossed over at about 2 years (-2.2%, -4.4-0.0%), and further indicated a borderline statistically significant 2.2% benefit with the invasive strategy (HR 0.93, 0.80-1.08, P=0.34)."
"There was no major difference in event-free survival, marked by the area between the curves," he added. “Investigators also found no significant difference for key pre-specified subgroups including age, sex, diabetes and even anatomic complexity.”
Post-hoc subgroup analysis using the modified Duke Prognostic Index also demonstrated a clear prognostic benefit with CABG and PCI for patients with triple-vessel CAD (≥70%) or double-vessel disease (≥70% including proximal LAD), Stone said.
A second subgroup analysis further showed significant prognostic improvement with PCI and CABG for patients with left ventricular dysfunction (EF 35-45%) or heart failure (NYHA Class I-II).
"As negative trials, these subgroup analyses remain only hypothesis-generating and require conservative assessment," Stone said. "But these results clearly show the prognostic benefits of invasive revascularization consistent with earlier CABG studies like STICH."
As for an optimal revascularization strategy, Stone emphasized weighing the pros and cons of each approach based on a recent meta-analysis published by Marc S. Sabatine, MD (Brigham Women's Hospital, Massachusetts, USA) and colleagues in the Lancet.
"Asking where to apply PCI asks what should be done in LM and multivessel disease," Stone said. "The recent meta-analysis that compared DES-PCI versus CABG in left main showed no significant difference in 5-year all-cause mortality but tradeoffs with each approach like CABG with lower mortality rates in high SYNTAX scores and lower 1-year stroke rates with PCI."
Regarding quality-of-life (QoL), two respective surveys on the SYNTAX and EXCEL trials showed similar long-term QoL outcomes between PCI and CABG, albeit a small early benefit with PCI stemming from reduced post-procedural physical limitations.
"PCI can improve survival for LM, HF, and reduced LVEF patients with stable CAD and extensive or symptomatic CAD," Stone said. “Importantly, primary PCI extends beyond stable CAD with benefits reported in ACS-STEMI for mortality, reinfarction, stroke or recurrent ischemia and NSTE-ACS for MI."
Edited by

Cheol Hyun Lee, MD
Keimyung University Dongsan Medical Center, Korea (Republic of)
Written by



Leave a comment